
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
The Psychological Impact of Foetal Loss at Term on Sudanese Mothers Volume 1 - Issue 3
Kunna A1, Khairy S Ismail2, 1, Hassan A Elkheir3*, Suad Enour1 and Umbeli Taha2
- 1Department of Obstetrics and gynecology, University of Bahri, Sudan
- 2Department of Obstetrics and gynecology, Omdorman Islamic university, Sudan
- 3Omdorman Maternity Hospital, Central laboratories, Sudan
Received: January 12,2018; Published: February 05,2018
*Corresponding author: Akram Elkhier Hassan, Omdorman Maternity Hospital, Central laboratories. Khartoum, Sudan
DOI: 10.32474/IGWHC.2018.01.000114
Abstract
This is a descriptive, cross-sectional study to explore and describe the psychological impact and social support following perinatal loss among Sudanese Mothers who have been through it before, hence, to evaluate it among them, to estimate the magnitude of psychological and social consequences of childbirth resulting in perinatal death, to explore and describe social support following perinatal loss, and to assess how well our health care providers feel when dealing with parents who have suffered perinatal loss. The study was conducted at 3 hospitals; namely, Saudi, Saad Abulilla and Omdurman maternity hospitals; among Sudanese Mothers who had experienced perinatal losses from February to July 2014, using a self- administered questionnaire after a prior informed consent. They were interviewed between the 1st days to 12 months following their fetal losses. Data was collected by trained data collectors- through self-administered questionnaires and interviews- using a structured format, and analyzed using Statistical Package for Social Science (SPSS) Program version 16 software. A total of 110 respondent Sudanese mothers were included, most of them were house wives, and 58(52.7%) aged between 31-40 years. 96 (87.3%) experienced sadness after loss and had a desire to carry another pregnancy in the future. Family and husband play an important role in providing support. 96 (87.3%) agreed that whatever happened was a test from God. Mothers who have been through perinatal losses should be screened for psychosocial impact. Family, husband and friends should continue to provide emotional support. Health care providers should provide psychosocial support during antenatal, delivery and postnatal care.
Keywords: Sudan; Prenatal Loss; Psychological
Introduction
Perinatal loss refers to "the death of an infant during pregnancy or soon thereafter". It's known to cause major emotional and psychological effects on mothers. However, little is known about these effects in developing countries. There are several different kinds of perinatal loss, including miscarriage, stillbirth, and neonatal death. Miscarriage also known as spontaneous abortion- is the body's natural termination of pregnancy before 20 weeks gestation (i.e. Mostly within the 1st 13 weeks). It's the most common form of Perinatal Loss, stillbirth, and neonatal death. A stillbirth is a fetal death that occurs after 20 weeks gestation, while, Neonatal Death occurs when an infant dies within 28 days following a live birth [1]. No doubt, the mother may experience feelings of extreme sadness and loss, when she receives the news that her baby has not survived. That's natural, for sure. Considering there is no such a right or a wrong way to feel. There are no "SHOULD(s)". She may feel betrayed, or even something went wrong with her. Perhaps, she is struggling to make meaning for her loss. The memory of this experience will linger, but try to have both courage and faith that, over time, such heartache will lessen somehow. At this stage of mother's life, it is important to let her mourn as she desires, and take as much time as she needs. One of the most helpful things she should have - at this time- is a strong network of support. Try to reach out to her friends and family. Talk to them about her feelings. Don't hesitate to ask them for helping her out whenever she needs [2]. Keeping in mind that others may not understand the magnitude of that loss. Consider explaining the significance of the loss to those who are close to her. Communicate with them, as much as you can, hence, you can help them sympathize and become better able to support her the way she needs [2]. In such difficult times, one can hardly cope alone. The mother may find that the experience brings her closer to her spouse. She may also find that the pain drives each of them to seek an "alone time", and that she feels herself growing apart.
One of the challenges of perinatal loss is the realization that the mother and her partner are grieving in different ways [2] You must not let this difference in mourning styles discourage them from attempting to communicate with each other. Remember, the partner is hurting, too. Take turns talking to each other about how they are feeling. Support each other [3]. If the mother has been through a perinatal loss before, subsequent pregnancies may be stressful. Hopefully; the odds are in her favor, as many as 85% of women who have experienced perinatal loss go on to have successful pregnancies. That means she has an excellent chance of conceiving again in the future [3].
The causes of many pregnancy losses are idiopathic. That's, many early-pregnancy losses are due to genetic issues those are rarely diagnosed. Anatomical abnormalities of the mother or fetus can also interfere with implantation, fetal growth, and development [4]. Pregnancy loss is very common; occur in more than an estimated 1 million women each year. Early losses, most commonly manifested during the first trimester, are estimated to occur in up to 25% of all conceptions. Late losses (i.e., after 20 weeks) occur in approximately 2%-4% of all pregnancies, in the form of stillbirths, preterm births, or neonatal deaths. There are some cases where treatments have been developed. However, the number of perinatal losses remains relatively stable and the rate of preterm birth (a frequent cause of neonatal death) continues to be alarmingly high. Although the stillbirth rate has decreased 10.7% in the last decade, in the developed country but in developing country still remaining high [4].
The loss of baby, either during pregnancy, or, after delivery holds great significance for parents and their close family members. This loss may be perceived as a loss of the parent's future, hopes, and of their potential for fulfilling their dreams [5]. It may also cause major emotional problems in adjustment during bereavement period. Feeling of unpreparedness to face the painful reality of the loss, denial, and feeling that their world no longer makes sense are commonly expressed. Every year, there are over 6.3 million perinatal deaths in the world, of which almost all occur in developing countries and 27% of them in the least developed countries alone (WHO, 2007). Stillbirths account for over half of all perinatal deaths. One third of all stillbirths take place during delivery and are largely avoidable [6]. According to annual report of stillbirth and neonatal deaths in 2005 reported that for 19982002, the largest proportion of all perinatal deaths were classified as normally formed, and macerated stillbirths. An Evidence-based study showed that perinatal loss significantly increases anxiety in a subsequent pregnancy and often produces feelings of guilt [6]. Intrauterine fetal death (IUFD), still birth or neonatal death increases the risk of experiencing anxiety and depression during the first following months compared with women with a live birth [7]. There are studies demonstrated that stillbirth as a major stressor associated with post-traumatic stress disorders (PTSD) [7]. These studies also mentioned that having a good emotional support after stillbirth may be protective factor for PTSD. Alternatively the birth of a healthy baby after the next pregnancy had a curative effect for PTSD Table 1.
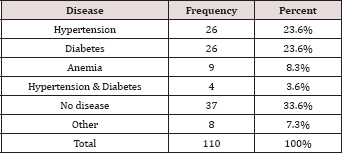
Table 1: Disease during pregnancy.
The risk of experiencing depression and posttraumatic stress disorder (PTSD) is prevalent during the next pregnancy, particularly when conception occurs soon after the loss [8]. As time elapses after bereavement, the degree of distress in mothers can gradually decrease [9]. A 30 month follow-up study on bereaved mothers noted a substantial reduction in the incidence of distress over the study period, from 21% at 2 months, 14% at 8 months to 10% at 30 months [4]. However, there is also evidence that some bereaved mothers suffer from long term psychological distress after such loss. For instance, a number of studies have documented that some bereaved women encounter long-term consequences including depression in subsequent pregnancies and prolonged grief reactions and marital disharmony that lead to separation and divorce [10]. Depressed mothers often felt guilty and ashamed at losing their unborn babies. Such women were often profoundly sad, cried, and yearned for their lost child. Although baseline depression status was associated with partnership breakdown, poor perceived support from partner at times of loss predicted subsequent partnership breakdown, as seen in a Swedish study that followed a cohort of women for 7 years after perinatal loss. The risk of partnership breakdown was 4 times higher among women with stillbirths compared to the women who had live babies [10]. An earlier study was carried out in rural Bangladesh indicated that perinatal death was one of the strongest predictors of postnatal depression [11]. Also, recent cross-sectional studies in Africa and in Malaysia indicate that around half of all women with perinatal death have high levels of depressive symptoms in the postnatal period [12,13].
Regarding social consequences, data shows that grieving parents also have to contend with a wide range of negative social effects following a perinatal death, such as isolation from friends, extended family members, and others in their social networks leaving them more emotionally vulnerable [14]. Over time, partners often experience increased difficulties in supporting each other due to gender differences in grief and coping, strained communication, and characteristic patterns of misunderstandings [14].
Factors significantly associated with higher depressive symptoms of perinatal losses were poor support from husband, friends, family and pregnancy complications and previous history of perinatal loss. A study reported that mothers who have been through perinatal loss expressed their wishes that people should acknowledge their losses, be considerate and sensitive, and give them a listening ear and emotional support. It was also mentioned in the study that health workers should provide the mothers with appropriate supports. Therefore, certain measures need to be taken to help those parents to cope with perinatal loss. Parents were encouraged to develop a birth planso that their special needs and concerns are more likely to be met [15] Table 2.
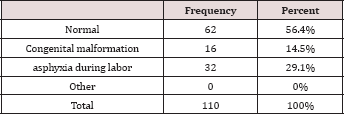
Table 2: Causes of baby death.
Health care providers must evaluate the significance of parent's perception on perinatal loss before starting an intervention; otherwise, their assumptions in giving care will cause additional pain to these parents [5]. A study showed that parents with previous losses had significantly higher antenatal anxiety on the outcome of the next pregnancy than the expectant parents with no history of perinatal loss [14,16]. Couples who experienced the death of a baby were significantly more likely to have one or both partners' distressed, compared to non-bereaved couples. Several large population-based studies related to psychological impact of perinatal loss have been conducted in many countries, but according to my knowledge there is no study conducted in Sudan Table 3.
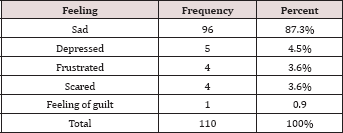
Table 3: Feeling after Perinatal Loss.
Methodology
In this descriptive, cross- sectional study, and conducted at Saudi, Saad Abulilla and Omdurman maternity hospitals from February to July 2014 in postnatal ward, post-natal clinic, and neonatal intensive care unit (NICU). A total of 110 mothers, who had experienced perinatal loss were selected randomly after a prior informed consent. The interviews were conducted between 1st days to 12 months following perinatal loss. Ethical clearance was obtained from the research and ethical review committees of Sudan Medical and Scientific Research Institute (SUMASRI), and the agreement for data collection from the Ministry of Health Khartoum State Directorate of Research. . Data was collected by trained data collectors- through self-administered questionnaires and interviews- using a structured format, and analyzed using Statistical Package for Social Science (SPSS) Program version 16 software.
Results
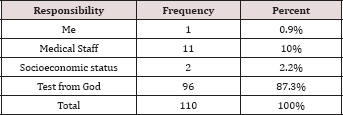
In this study, 110 respondent Sudanese Mothers were included for exploring and evaluating the psychological impact of fetal loss at term on them. Their ages are less than 50 years. A majority of them were house wives, and aged between 31-40 years 58(52.7%), teenagers were 16 (14.6%), 25 (22.7%) were between 20-30 years old, and 11 (10%) were above 40 years of age. However, about one third of them were primigravidae (i.e. lost their 1st babies) and were 37 (33.6%), while the respondents lost their 2nd babies were as equal as those lost their 3rd babies and each were 28 (25.5%). Similarly, 37 (33.6%) had no underlying medical problem during pregnancy, 26 (23%) had hypertension (i.e. either essential or PIH), 26 (23.3%) had diabetes (i.e. either diabetes mellitus or gestational diabetes), and very few had anemia (i.e. 9 (8.3%)) and other condition (i.e. 8 (7.3%)) e.g. malaria. A majority of them had an antenatal checkup from specialists (75.4%). Also, 94.5% had a regular antenatal checkup. Most of the deaths were normally formed 62 (56.4%), and 32 (29.1%) deaths caused by asphyxia during labor followed by congenital malformation 16 (14.5%). A majority of the deaths were during 38—40 weeks (58.2%) most of them were macerated still birth. Mothers experienced sadness after Loss were 96(87.4%), while few of them being depressed, frustrated and scared. A majority of the respondent claimed that the responsibility of their baby loss were test from god (86.9%) and few due to medical staff mistakes and very few due to socioeconomic status, and just one blame herself Tables 4 & 5.
Table 4: Shows majority of the respondent received support from husband and family after perinatal loss (51.8%) and very few from medical staff.
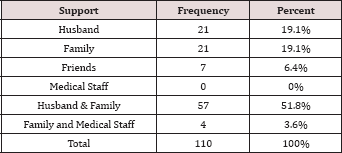
Table 5: Who is responsible for baby loss.
Discussion
Perinatal loss has a great impact on any woman that psychosocial support at this time is of a great importance. This is a descriptive, cross-sectional study, explores the impact of perinatal deaths on women's psychological and social life. The results indicate that such women experience increased rates of psychological distress and suffer from negative social consequences that persist up to 6 months after the perinatal death. Some shared the same experiences and others differed but it could be related to their social background knowledge on outcome of pregnancy. The present study has shown that mothers who experienced perinatal loss felt sadness, depressed, frustrated and scared. Other studies also mentioned that the majority of mothers experiencing perinatal loss felt sadness being depressed, confused and having nightmares [15]. Another study mentioned that people suffering perinatal loss expressed their wish that people would acknowledge their loss, be considerate and sensitive, and lent a listening ear and emotional support [6] this study shown that the family and husband support play important role in reducing the psychological distress among mothers who experienced perinatal loss and help them to cope with the loss .Other studies mentioned that the need for psychosocial support from friends was found to be significant. It stated that friends should help relatives, siblings of the dead baby, and others who are close to the parents during bereavement period. Support is often viewed as the most credible when it comes from someone who has previously experienced and successfully managed a similar crisis.. Also, the study showed there was a little support from health care provider; other study mentioned that parents perceived many healthcare provider behaviors to be thoughtless or insensitive [11]. A study showed that there is a relationship between maternal health condition during pregnancy, fetal condition, high maternal age and perinatal loss also another study mentioned that previous history of perinatal loss, higher maternal age, low socioeconomic status, and poor maternal and fetal health conditions were significantly related [8]. However, other studies have reported that there were no significant relationships in depressive state of mothers among the following factors: previous perinatal loss, maternal age, total income, maternal educational level, race, occupation, maternal health condition, obstetric history, and fetal condition. Other studies mentioned that Factors which have been reported to increase the risk of adverse psychological outcomes for parents following a perinatal death include: perceived inadequate social support, traumatic circumstances surrounding the death, difficulties in coping with a crisis, problematic relationships in the nuclear family and the presence of other life crisis [7]. Almost all the mothers in the study were Muslim, and majority of them answers that what happen to them were test from God. Other study also showed that, the religious practice improved mothers' perception of perinatal loss. A strong religious background made them feel better [13].
Conclusion
In conclusion, every mother experiencing a perinatal loss showed some level of psychological impact which affected their feelings but the role of family, husband and health care provider support was also found to play a major role. This study showed that a majority of the mothers who had perinatal loss are house wives who are highly educated. Hence, they need to be both physically and mentally well. In addition to that, this study also showed that husband and family play a significant role in supporting mothers who had been through perinatal loss, where by those who received support from husband and family were less stressed. Almost all respondent were Muslim. Majority of the mothers experienced sadness after loss. Despite these emotions, majority still had a desire to carry another pregnancy in the future and they take the perinatal loss as a test from God.
Acknowledgement
The authors extend their thankfulness and gratitude to all individuals and institutes contributed in this research. Special thanks to Sudan Medical and Scientific Research Institute (SUMASRI), the Ministry of Health Khartoum State Directorate of Research, Saudi, Saad Abulilla and Omdurman maternity hospitals.
References
- Jorde L, Carey J, Neurological MB (2013) undefined. an Overview: Clinical Diagnosis and Types of Genetic Disorders With Representative Clinical Examples. Books Google Com. 2013.
- Doyle CS (2011) When Delivery Expectations Change. Nurs Womens Health 15(6): 465-469.
- Simkin P, Whalley J, Keppler A, Durham J, Bolding A (2016) Pregnancy, Childbirth, and the Newborn: The Complete Guide (5 th Edition).
- Gausia K, Fisher C, Ali M, Oosthuizen J (2009) Magnitude and contributory factors of postnatal depression: A community-based cohort study from a rural sub district of Bangladesh. Psychol Med 39(6): 999-1007.
- Armstrong D (2001) Exploring Fathers' Experiences of Pregnancy After a Prior Perinatal Loss. MCN. Am J Matern Nurs 26(3):147-153.
- Blackmore ER, Cote-Arsenault D, Tang W, Glover V, Evans J, et al (2011) Previous prenatal loss as a predictor of perinatal depression and anxiety. Br J Psychiatry 198(5): 373-378.
- Hughes PM, Turton P, Evans CDH (1999) Stillbirth as risk factor for depression and anxiety in the subsequent pregnancy: cohort study. BMJ 318(7200): 1721-1724.
- Janssen HJ, Cuisinier MC, Hoogduin KA, de Graauw KP (1996) Controlled prospective study on the mental health of women following pregnancy loss. Am J Psychiatry 153(2): 226-230.
- Turton P, Hughes P, Evans CD, Fainman D (2001) The incidence, correlates and predictors of post traumatic stress disorder in the pregnancy after stillbirth. Br J Psychiatry 178: 556-560.
- Sutan R, Amin RM, Ariffin KB, Teng TZ, Kamal MF, et al. (2010) Psychosocial impact of mothers with perinatal loss and its contributing factors: an insight J Zhejiang Univ Sci B 11(3): 209-217.
- Adeyemi A, Mosaku K, Ajenifuja O, Fatoye F, Makinde N, et al. (2008) Depressive Symptoms in a Sample of Women Following Perinatal Loss. J Natl Med Assoc 100(12):1463-1468.
- de Montigny F, Beaudet L, Dumas L (1999) A baby has died: the impact of perinatal loss on family social networks. J Obstet Gynecol Neonatal Nurs 28(2): 151-156.
- Wallerstedt C, Lilley M, Baldwin K (2003) Interconceptional counseling after perinatal and infant loss. J Obstet Gynecol Neonatal Nurs 32(4): 533-542.
- Hutti MH (2002) Parents' perceptions of the miscarriage experience. Death Stud 16(5): 401-415.
- Armstrong DS (2002) Emotional Distress and Prenatal Attachment in Pregnancy After Perinatal Loss. J Nurs Scholarsh 34(4): 339-345.
- Kamwendo F, Forslin L, Bodin L, Danielsson D (2000) Epidemiology of ectopic pregnancy during a 28 year period and the role of pelvic inflammatory disease. Sex Transm Infect 76(1): 28-32.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...















